>>Return to CareNet Information
November is “Antimicrobial Resistance (AMR) Awareness Month” in Japan, and November 18 to 24 is designated as “World Antimicrobial Awareness Week.”
AMR occurs when bacteria, viruses, fungi, and parasites change over time and become unresponsive to medications, making it more difficult to treat infections and increasing the risk of disease spread, severity, and death. It is essential that antimicrobials are used with caution and prescribed appropriately. The World Antimicrobial Awareness Week is a campaign based on a global action plan to address the growing problem of resistance to antibiotics and other antimicrobials.
AMR is a global issue causing numerous deaths. In Japan, the AMR Clinical Reference Center reported in 2019 that bacteremia such as methicillin-resistant Staphylococcus aureus (MRSA) and fluoroquinolone-resistant E. coli (FQREC) resulted in approximately 8,000 deaths, highlighting the significant impact of AMR.
https://amr.ncgm.go.jp/pdf/20191205_press.pdf(Japanese)
In conjunction with this global and Japanese campaign against AMR, CareNet conducted a survey of 203 of its physician members who treat infectious diseases, including general internal medicine and otorhinolaryngology, who deal with upper respiratory tract infections, regarding their awareness of antimicrobial treatment. The results revealed the following points:
<Survey period>10/9/2023 – 10/16/2023
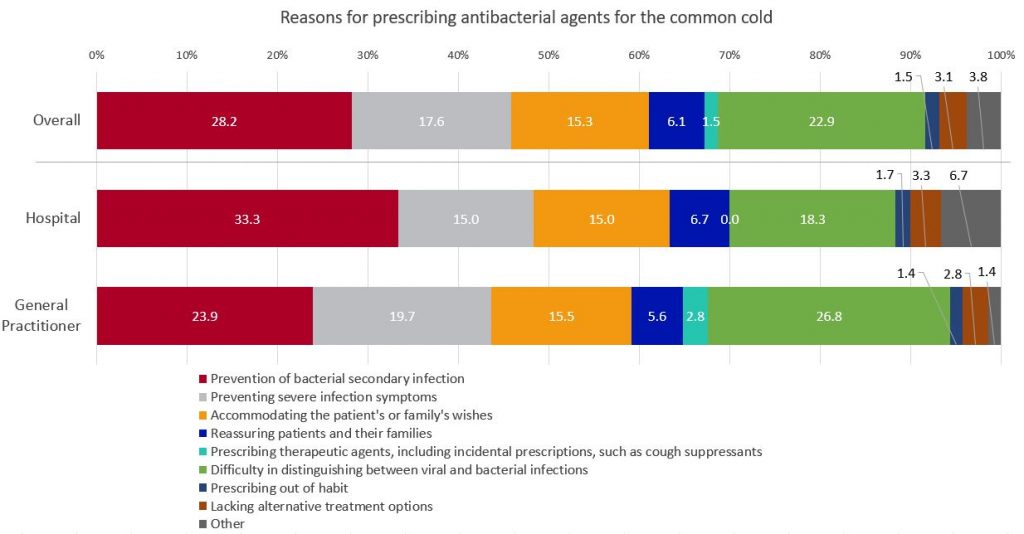
・The primary reason that patients exhibiting upper respiratory tract symptoms without an underlying disease are diagnosed with a common cold and prescribed antimicrobials was “difficulty in distinguishing between viral and bacterial infections” and “prevention of secondary infections.”
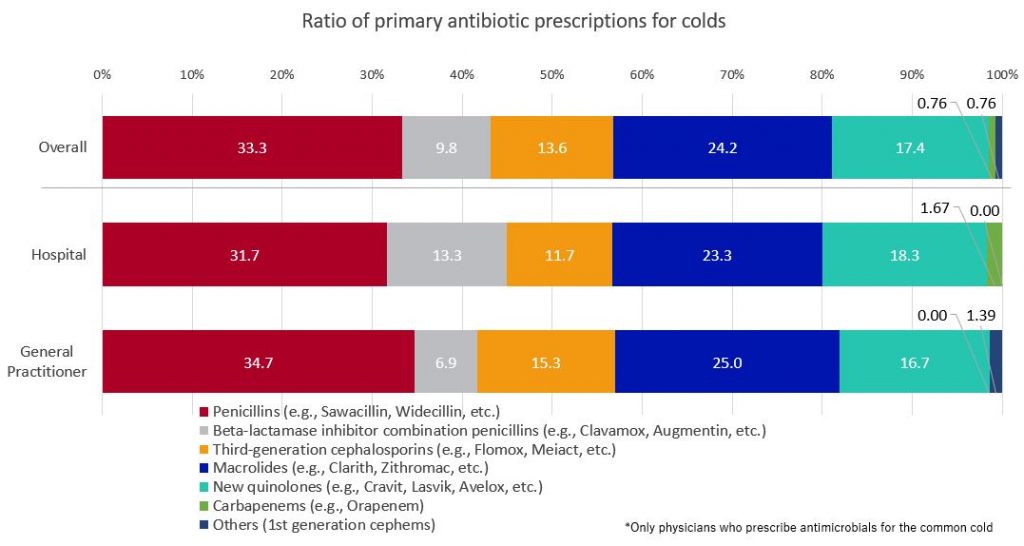
・Penicillins(e.g., Sawacillin, Widecillin, etc.) are the most commonly prescribed antimicrobials for primary treatment of the common cold, followed by macrolides.
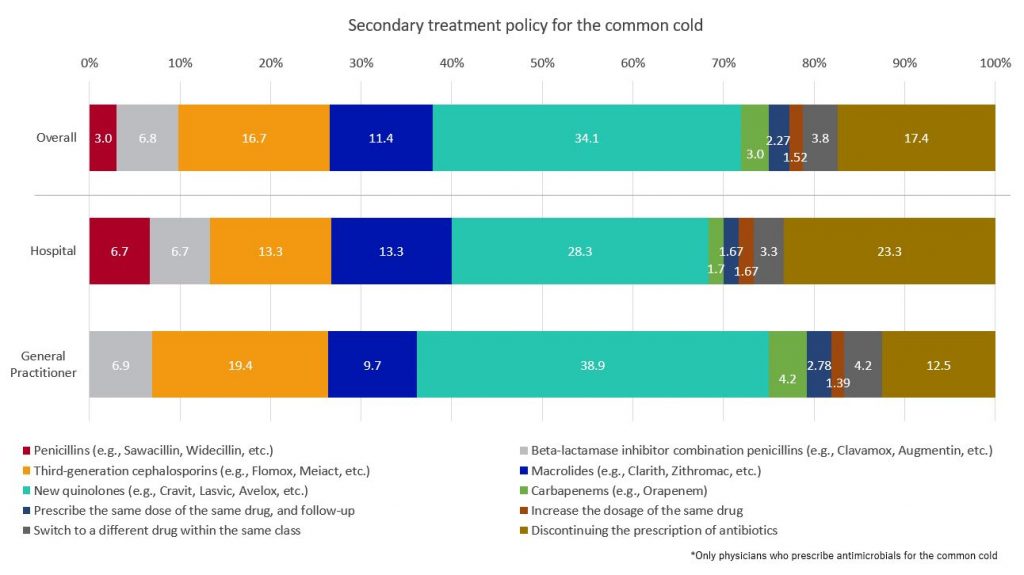
・Policies for secondary treatment, when no effect was observed after prescribing antibiotics as the primary treatment for the common cold, varied based on the size of the medical facilities. Physicians at facilities with more than 200 beds most commonly prescribe “new quinolones” (e.g., Cravit, Lasvik, Avelox, etc.), followed by “discontinuing the prescription of antibiotics.” In facilities with fewer than 200 beds, “new quinolones” are also the most prescribed, but the second most common choice is “third-generation cephalosporins” (e.g., Flomox, Meiact, etc.).
【Key Findings】
The primary reason for diagnosing a cold and prescribing antibiotics to patients with upper respiratory symptoms who do not have an underlying disease is the “prevention of bacterial secondary infection” (28.2%), with the next most common reason being “difficulty in distinguishing between viral and bacterial infections” (22.9%). Among facilities with 200 or more beds, 33.3% cited “prevention of bacterial secondary infection” as the main reason, while in facilities with fewer than 200 beds, 26.8% reported “difficulty in distinguishing between viral and bacterial infections.”
[Table1]
When using antibiotics as the primary treatment for the common cold with, “penicillins” (e.g., Sawacillin, Widecillin, etc.) are the most frequently prescribed, accounting for 33.3% of prescriptions, while “macrolides” (e.g., Clarith, Zithromac, etc.) followed at 24.2%.
[Table2]
When the primary treatment for the common cold proved ineffective, 34.1% of the respondents chose “new quinolones” (e.g., Cravit, Lasvic, Avelox, etc.) as their alternative treatment strategy, with “discontinuing the prescription of antibiotics” second, at 17.4%. Physicians from larger facilities with over 200 beds exhibited a similar pattern to the overall trend. However, among physicians in smaller facilities with fewer than 200 beds, the most common choice was “new quinolones” at 38.9%, with “third-generation cephalosporins” (e.g., Flomox, Meiact, etc.) as the second choice, at 19.4%.
[Table3]
>>Return to CareNet Information


Comments are closed